The emergence of the delta variant of SARS-CoV-2 (which causes COVID-19) earlier this year was not a surprise and has resulted in an additional uptick in morbidity and mortality across the world. Studies indicate a high effectiveness of many vaccines designed for the previously dominant alpha variant, but we are still waiting for the full story on the delta variant.
English researchers recently published an observational study using a test-negative case-control design to estimate the effectiveness of the Pfizer and AstraZeneca vaccines against the delta strain compared to the alpha strain. Test-negative case-control studies have been popularized in the last 10 or so years as a way to study effectiveness of different kinds of pneumococcal and influenza vaccines. The method looks at groups presenting with similar symptoms and compares those who test positive for the variant in question with those who test negative (but may have another variant of the same disease). In this particular study, authors compared people with COVID-like symptoms and confirmed delta infection (“cases”) and two separate symptomatic control populations –– those with negative testing and those with the alpha variant.
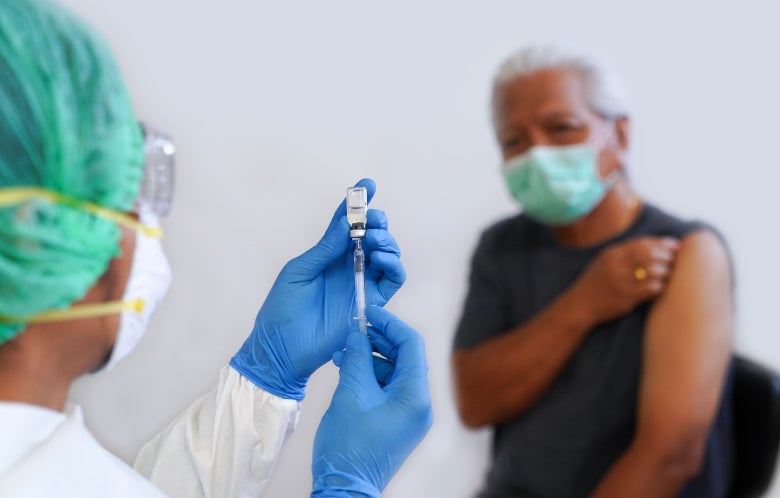
English patients with symptoms compatible with COVID-19 were enrolled during a seven-week period, including a mix of people who were unvaccinated, partially-vaccinated, and fully-vaccinated with either an mRNA-based vaccine (Pfizer) or an adenovirus-vectored vaccine (AstraZeneca). More than 100,000 control patients who tested negative were included along with 19,109 patients who had positive COVID-19 testing with gene sequencing confirming the presence of alpha or delta variant. A week-by-week breakdown of the test status in one of the tables allows us to watch the percentage of COVID-19 cases caused by the delta variant to grow from 0.5 percent in the first week to 63 percent by the 7th week of the study.
After only one dose of the vaccine, adjusted effectiveness was only 48 percent against alpha and 36 percent against delta for the Pfizer vaccine and 49 percent and 30 percent respectively for AstraZeneca. Effectiveness improved significantly after the second dose for Pfizer (adjusted 94% against alpha and 88% against delta) and a little bit less so for AstraZeneca (75% against alpha and 67% against delta). Results were similar in a secondary analysis that estimated vaccine effectiveness against delta by aligning the proportion of delta cases with vaccination status, a method that relies on the assumption that if the vaccines were less effective against the delta variant, delta would make up a higher percentage of cases.
Getting into the nitty-gritty of relative vaccine effectiveness is fascinating and has important policy implications, but since this is the EBM Focus, we’d like to discuss the potential implications of collider bias, a type of selection bias that occurs in observational studies. Collider bias is represented visually by variables colliding together and changing the linear path to an outcome. In a hypothetical example from this study, contracting the delta variant (more common with foreign travel) and getting the Pfizer vaccine (more common in healthcare workers) each may reflect a population with different characteristics than the general population; when these two factors occur together, vaccine effectiveness may also be different than if neither or only one of those risk factors were present. In this observational study restricted to symptomatic people, vaccination status and virus variant might “collide” at the outcome of those seeking medical care for symptoms, skewing estimates of vaccine effectiveness. When present, collider bias limits the ability of a study to answer questions about the population as a whole (including asymptomatic patients and those who have symptoms but don’t seek medical care) and is a limitation of the otherwise nifty test-negative case-control method.
For more information, see the topic COVID-19 (Novel Coronavirus) in DynaMed.