Prior to the COVID-19 pandemic, tuberculosis (TB) was the world’s leading cause of death from a single infectious agent. While TB is now the second leading cause of death, behind only COVID-19, it remains an important global public health threat causing an estimated 10 million cases and more than one million deaths each year.
TB is caused by Mycobacterium tuberculosis, which is spread when an infected person coughs up airborne particles (droplet nuclei that contain the organisms) that are breathed in and enter the airway of an uninfected person. In most persons who become infected, the result is latent TB infection (LTBI) rather than TB-causing disease. In the absence of HIV or other significant immunocompromise, only five-10 percent of people with the latent form LTBI develop TB disease in their lifetime.
According to the 2023 WHO Global Tuberculosis Report, there were 7.1 million newly diagnosed cases of TB disease reported in 2019. During the first two years of COVID-19 pandemic, this dropped to 5.8 million and 6.4 million cases for 2020 and 2021, respectively. Unlike other respiratory infectious diseases that declined largely due to pandemic-related safety measures that limited transmission, the substantial decrease in reported TB cases was most likely due to pandemic-related disruptions. These systemic disruptions affected access to, and provision of, TB services, which in turn impacted the ability to diagnose, treat, and report new TB cases. In other words, while there was a decrease in the detection and treatment of new TB cases reported during the pandemic, the number of people developing TB may have actually INCREASED due to pandemic-related disruptions of TB control.
By 2022, the number of reported newly diagnosed TB disease cases reached 7.5 million, the highest number since the WHO began global TB monitoring in 1995. This increase reflects a backlog of cases from the first two years of the pandemic when TB services were interrupted. Delayed diagnosis and treatment due to service disruptions meant greater TB transmission and an increase in TB deaths. The figure from WHO displays this, showing that there were almost 500,000 excess TB deaths between 2020 and 2022 compared with the number that would have occurred if pre-pandemic trends in TB control had continued without interruption.
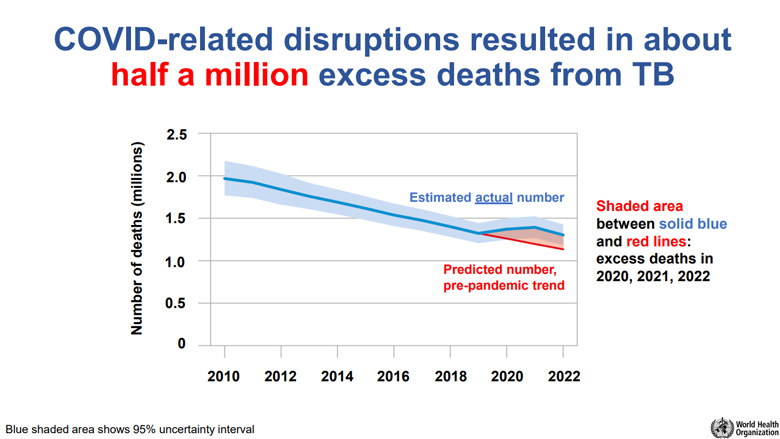
World Health Organization Global Tuberculosis Report 2023: Estimated number of excess TB deaths during the COVID-19 pandemic and its aftermath. The blue shaded area represents the 95% uncertainty interval of the action number of deaths estimated to have been caused by TB; the red line shows the estimated number of deaths that would have been caused by TB in the absence of the COVID-19 pandemic; the red shaded area shows the excess number of deaths caused by TB due to disruptions associated with the COVID-19 pandemic.
The WHO End TB Strategy established in 2015 calls for 75 percent reduction in TB deaths and 50 percent reduction in TB incidence by 2025. As of 2022, the net reduction in global deaths was 19 percent and incidence was 8.7 percent, far from the aspirational milestones set in 2015. While the increased number of reported cases can be taken as an indication that TB programs are recovering from pandemic-related disruptions, global TB targets for number of people treated for TB, number of people initiated on TB preventive treatment and funds available for provision of TB diagnosis, treatment and prevention are off track.
Ending the global epidemic of TB, a treatable and preventable disease, requires that new and reaffirmed commitments to the WHO End TB Strategy milestones and targets are urgently translated into action.



